
Humzah Iqbal1*, Hasib Haidary2, Hussein Riza3 and Haroon Iqbal4
1Department of Internal Medicine, University of California San Francisco, Fresno, CA, USA.
2American University of Antigua College of Medicine, Osbourn, Antigua & Barbuda.
3St. George’s University School of Medicine, True Blue, Grenada.
4University of California Irvine, CA, USA.
*Corresponding author: Humzah Iqbal, Department of Internal Medicine, University of California San Francisco, Fresno, CA, USA.
Received date: December 07, 2022
Accepted date: December 15, 2022
Published date: December 20, 2022
Citation: Humzah Iqbal, Hasib Haidary, Hussein Riza and Haroon Iqbal. (2022) “The Effect of Bariatric Surgery on Obesity–Related Hypersomnolence: A Literature Review”, J of Gastroenterology and Hepatology Research, 3(3); DOI: http;//doi.org/12.2022/2.10136
Copyright: © 2022 Humzah Iqbal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Background:
Bariatric surgery is a validated treatment modality for severe obesity with many beneficial effects on comorbidities of patients. The effects of surgical weight loss on obesity-related hypersomnolence and daytime sleepiness independent of sleep apnea have not been well studied. We aim to determine whether bariatric surgery leads to a decrease in hypersomnolence in patients with severe obesity.
Methods:
An extensive literature search was conducted using PubMed, Embase, Cochrane library, and Google Scholar through September 2022. Clinical trials published in English that assessed daytime sleepiness in patients with obesity before and after bariatric surgery were included.
Results:
A total of fifteen studies were included in the final analysis. These studies evaluated 1,166 patients with obesity, with an average pre-surgery body mass index (BMI) of 51.1 kg/m2 and Epworth Sleepiness Scale (ESS) score of 9.8. Most studies found a statistically significant decrease in ESS scores after surgery. Patients were reassessed at an average of 6.6 months after surgery with a mean post-surgical BMI of 36.4 kg/m2 and ESS score of 5.5 (p < 0.001). There was no significant correlation between the change in BMI and the change in ESS.
Conclusion:
Bariatric surgery can help to improve excessive daytime sleepiness in obesity. Patients undergoing surgical weight loss can see an improvement in BMI and ESS scores about 6 months following the intervention. However, the amount of weight loss is not predictive of the amount of improvement in hypersomnolence in this population.
Introduction:
Obesity is a worldwide epidemic with increasing prevalence around the globe. According to the World Health Organization (WHO), approximately 13% of adults suffer from obesity, which is defined as a body mass index (BMI) of > 30 kg/m2. [1] Obesity can trigger the development of various other comorbidities including dyslipidemia, type 2 diabetes mellitus, cardiovascular disease, gallbladder disease, respiratory disorders, and sleep apnea. [2] Obstructive sleep apnea (OSA) is a syndrome of disordered breathing that results from an obstruction of the upper airways during sleep. [3] Obesity is the greatest risk factor for developing OSA, and the relationship between the two conditions has been well documented in the literature. [4] Excessive daytime sleepiness (EDS) is another condition that is associated with both OSA and obesity. EDS is defined by the Epworth Sleepiness Scale (ESS), which is a subjective eight-question questionnaire that accurately and reliably estimates daytime sleepiness in adults. [5] Scores ≥ 10 signify the presence of EDS while scores ≤ 6 signify lower than average daytime sleepiness. EDS and hypersomnolence in obesity is often thought to be a direct result of associated sleep apnea. However, multiple studies have demonstrated a weak relationship (r < 0.3) between the severity of OSA and the severity of hypersomnolence. [6-9] Additionally, 30% of patients with severe obesity and OSA were shown to have persistent hypersomnolence despite high levels of continuous positive airway pressure (CPAP) > 7 hours/night. [10] Hypersomnolence and EDS in obesity is not solely due to OSA, but rather related to other factors independent of sleep apnea, though the exact mechanisms are unclear. One proposed mechanism involves the upregulation of somnogenic hormones and adipokines and concurrent downregulation of alerting substances in response to a high-fat and high-sugar diet as well as an increase in adipose tissue. [11]
Treatment of obesity involves several lifestyle modifications and pharmacologic agents which have proven to be somewhat effective in mild to moderate cases. However, patients with severe obesity, defined as a BMI > 35 kg/m2 often require surgical intervention. Bariatric surgery has been shown to be a viable treatment option with positive effects on the comorbidities associated with severe obesity. [12] Options for surgical intervention include laparoscopic sleeve gastrectomy (LSG), laparoscopic gastric bypass (LGB), and intragastric balloon (IB). Bariatric surgery has been shown to improve OSA in most cases, defined as an improvement in the apnea-hypopnea index (AHI). [13] Multiple clinical trials and systematic reviews have demonstrated this effect, regardless of the type of surgery. [14] However, there remains a paucity of systematic reviews assessing the effect of bariatric surgery on obesity-related hypersomnolence and EDS, as a factor independent of OSA.
Methods:
Search Strategy and Criteria:
A literature search was employed using PubMed, Embase, Cochrane library, and Google Scholar databases from inception through September 2022. The search query used in this review was (“bariatric” OR “weight loss” OR “surgery” AND “hypersomnolence” OR “sleepiness” OR “Epworth”). Studies were independently reviewed and screened for eligibility. Included articles were required to be clinical trials published in English that demonstrated data in patients with severe obesity before and after undergoing bariatric surgery. Full text articles were then reviewed and excluded if they did not report pre and post-surgical BMI and ESS scores or the time to follow up. Any discrepancies were resolved by discussion.
Outcomes and Data Extraction:
The data extracted from each study included the first author, year of publication, country, number of patients included, mean age of patients, type of bariatric surgery, mean BMI before and after intervention, mean ESS score before and after intervention, and the mean time to follow up after intervention. The primary outcome was the level of daytime sleepiness, defined as mean ESS score (0-24), before and after the surgical intervention. The secondary outcomes were the mean BMI before and after the intervention, as well as the time to follow up, defined as the length of time after surgery at which the repeat data was obtained.
Results:
A total of fifteen studies met the criteria and were included in the final analysis. These articles consisted of independent cohort studies and case-control studies which examined a total of 1,166 patients. A summary of the data is represented in Table 1. Only two studies had < 20 patients and eight had > 40 patients. The mean age of patients included in the study was 42.8 ± 6.9 years. Fourteen of the studies employed LSG and/or LGB while one study had IB as the intervention of choice. Fourteen studies showed a statistically significant decrease in ESS scores pre and post-surgery, while one study found no significant difference. The mean ESS score before bariatric surgery was 9.8 ± 2.5 and 5.5 ± 1.8 after surgery. All fifteen studies included in this review found a statistically significant decrease in BMI pre and post-surgery. The mean BMI before bariatric surgery was found to be 51.1 ± 2.1 kg/m2 and 36.4 ± 1.9 kg/m2 after surgery. The mean time to follow up was 6.6 ± 0.6 months. The pooled results revealed a mean decrease in BMI of 14.7 kg/m2 and a mean decrease in ESS score of 4.3 across all studies. The correlation between improvement in BMI and improvement in ESS score was weak (r = 0.22). Additionally, the time to follow up and improvement in ESS score were also found to be weakly correlated (r = 0.27). All results from this review were statistically significant (p < 0.001).
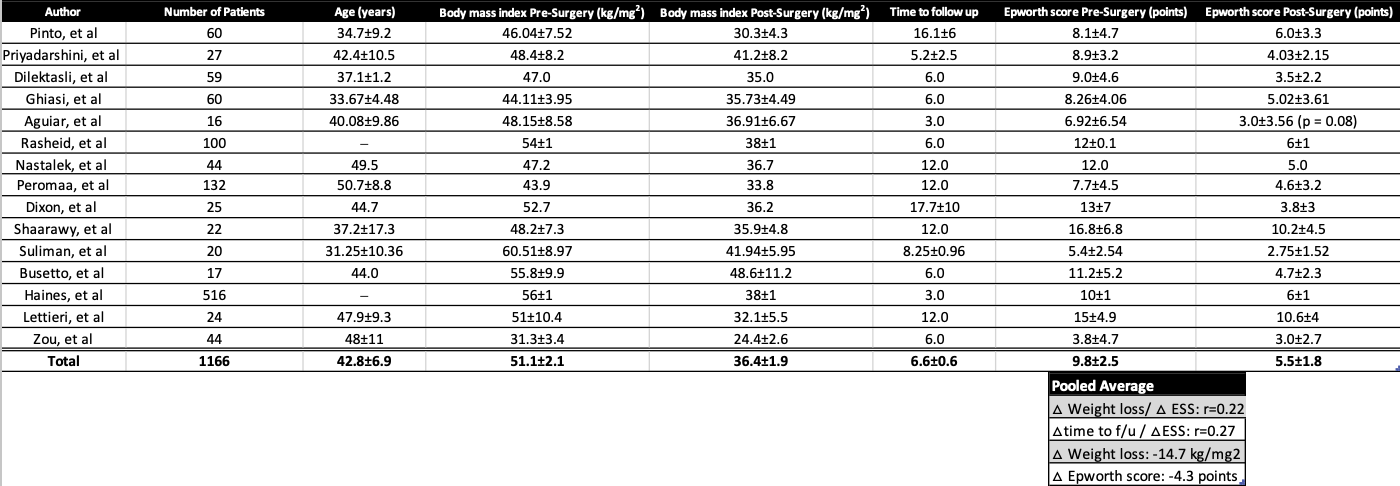
Table 1. Summary of data
Discussion:
This review highlights the effects of bariatric surgery on obesity-related hypersomnolence. We found a statistically significant decrease in the mean ESS scores an average of 6.6 months after surgery as compared to before surgery. This improvement was accompanied by a statistically significant improvement in BMI, though the degrees of improvement for the two outcomes were not strongly correlated.
The relationship between OSA and obesity has been well-documented, and obesity-related hypersomnolence has often been attributed to being an effect of sleep apnea. However, multiple studies have shown obesity-related hypersomnolence to be independent of OSA. [11] Our study found that the average decrease in ESS score following bariatric surgery for treatment of obesity was 4.3 points. However, a meta-analysis performed by Patel et al [16] found an improvement of only 2 points following CPAP therapy for OSA. Additionally, EDS has been shown to be common in patients with obesity in the absence of OSA. [17] In a study performed by Vgontzas et al [18], over 50% of non-apneic subjects with severe obesity and without OSA, other sleep disorders, or obesity hypoventilation reported significant daytime hypersomnolence; while only 2% of non-apneic controls without obesity reported daytime sleepiness. Several mechanisms have been proposed to explain this relationship. One mechanism proposed by Panossian et al [11] illustrates that serum levels of glucose, insulin, leptin, cholecystokinin (CCK), peptide YY, and enterostatin increase in response to consumption of a high-fat and high-sugar diet. These substances have been shown to exhibit somnogenic effects when present in the systemic circulation. Furthermore, the increased mass of adipocytes seen in obesity leads to an increase in levels of tumor necrosis factor-α (TNF-α), interleukin-6, and leptin. These substances impair alertness and wakefulness by modulating orexin, serotonin (5-HT), and noradrenergic signaling, which corresponds with findings of increased sympathetic nervous system (SNS) activity in obesity. [11] Another potential mechanism that can contribute to hypersomnolence in obesity is the presence of depression and other psychogenic factors. Obesity has been found to have an association with symptoms of depression and psychological disturbance. [19] A study performed by Bixler et al [20] found that depression was the greatest risk factor for developing EDS. Several other studies have been performed which also demonstrated an association between depression and hypersomnolence in patients with obesity. [21-22] A third proposed mechanism is the presence of increased insulin resistance. Two independent studies by Barcelo et al [23] and Nena et al [24] found an association between degree of insulin resistance and EDS in their subjects. However, other studies have found no significant association, and the mechanism remains unclear. [25]
Bariatric surgery is a proven method of achieving weight loss and a significant reduction in morbidity and mortality in patients with severe obesity. [26-28] Our study found that surgical weight loss also led to a significant improvement in daytime sleepiness and hypersomnolence. Though the mechanisms are unclear, bariatric surgery has been shown to improve several of the proposed physiologic etiologies of obesity-related hypersomnolence. A meta-analysis performed by Buchwald et al [29] demonstrated that bariatric surgery not only resulted in effective weight loss, but also in resolution of diabetes, hyperlipidemia, and hypertension in a substantial majority of patients, exhibiting an improvement in circulating glucose and insulin, insulin resistance, dyslipidemia, and SNS activity. Additionally, bariatric surgery has been shown to lead to a significant improvement in depressive symptoms, with the degree of weight loss strongly correlated with the degree of depression resolution. [30-31]
Several mechanisms exist to explain the positive effects that surgical weight loss can have on EDS and hypersomnolence in obesity irrespective of OSA. Though we demonstrated an improvement in EDS following surgery, the degree of improvement was not related to the amount of weight loss or amount of time that had passed after surgery. We can conclude that based on our study, bariatric surgery can improve obesity-related hypersomnolence. However, further studies are necessary to elucidate the exact mechanisms of this effect and the pathophysiology driving EDS in severe obesity.
Conflicts of interest:
The authors declare no conflict of interest.
Acknowledgements:
None to report.
Author contributions:
HI*, HH, HR, HI reviewed the literature and were involved in data extraction. HH, HR, HI aided in statistical analysis. HI* drafted the manuscript and revised it for important intellectual content. HI*, HH, HR, HI were involved in the review of the manuscript and final approval of the version to be published. HI* is the article guarantor.